A nursing care plan for hypertension is a structured framework for nurses to assess, diagnose, and manage high blood pressure effectively. Its goal is to prevent complications and support better patient outcomes through evidence-based care.
A complete plan includes five key elements: nursing assessment, diagnosis, expected outcomes, interventions, and evaluation.
At EssayPro, we provide help with nursing assignments for students like yourself, including the nursing care plan for hypertension. Our experts guide you through every stage, ensuring your work meets academic and clinical standards.


What Is Hypertension?
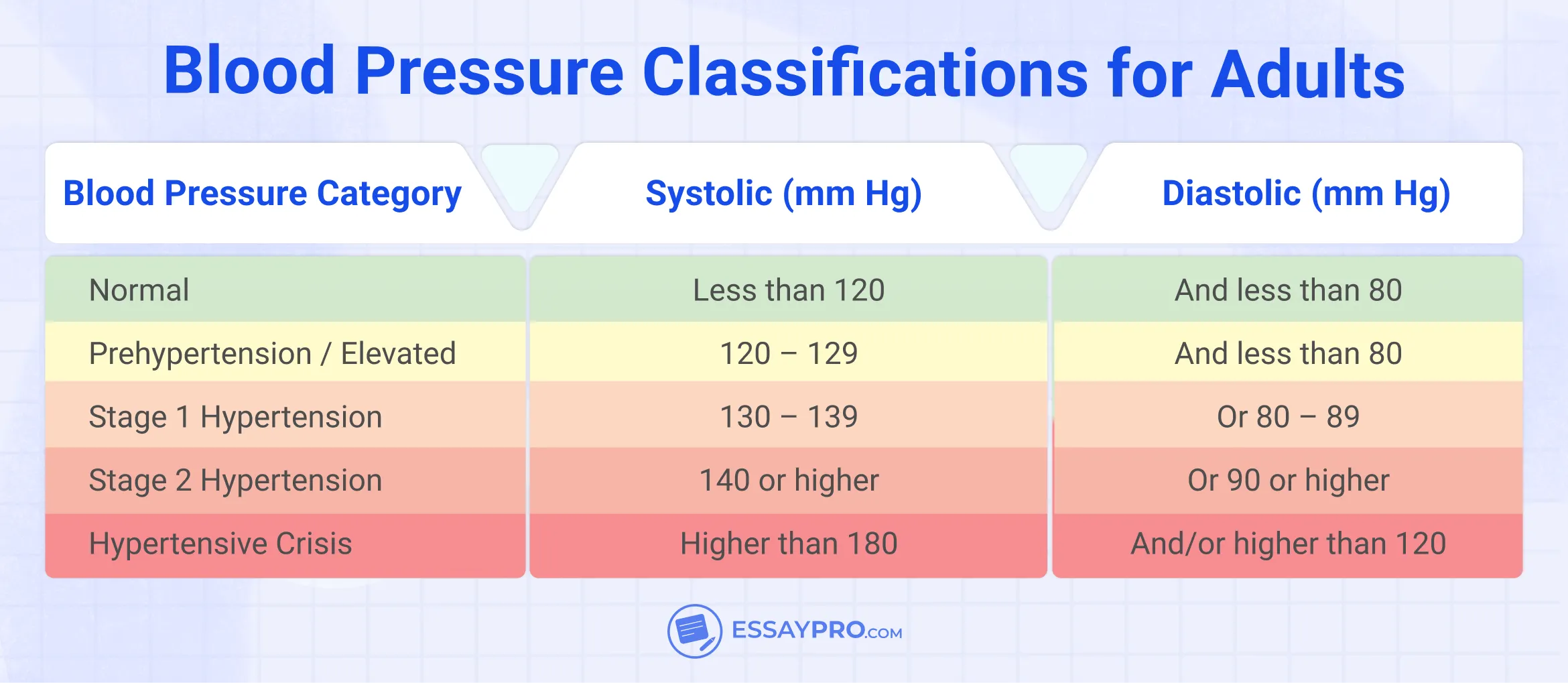
Hypertension, or high blood pressure, occurs when blood consistently pushes too forcefully against artery walls. Over time, this extra pressure makes the heart work harder and strains blood vessels, which can lead to heart failure, kidney damage, or stroke. An effective HTN care plan identifies the cause, monitors blood pressure regularly, and uses lifestyle or medical interventions to maintain control.
Hypertension Risk Factors
Hypertension builds up slowly, often because of daily choices or ongoing conditions. Some risks can be changed, while others can only be managed. Nurses help patients understand which apply to them and how to lower the chances of complications.
Common risk factors include:
- High salt intake that increases fluid retention
- Limited physical activity or a sedentary lifestyle
- Chronic stress that keeps blood pressure elevated
- Excessive alcohol use or smoking habits
- Family history of high blood pressure
- Age-related changes in blood vessels
Hypertension Signs and Symptoms
Hypertension often causes no noticeable signs until pressure reaches dangerous levels. That’s why nurses emphasize routine monitoring and patient awareness. When symptoms do appear, they may include:
- Headaches that come and go
- Dizziness or blurred vision
- Chest pain or tightness
- Shortness of breath during activity or rest
- Fatigue or feeling weak
Elements of a Hypertension Nursing Care Plan
A nursing care plan for hypertension follows the nursing process that is often called ADPIE: Assessment, Diagnosis, Planning, Intervention, and Evaluation.
- Assessment: Involves understanding your patient's situation clearly. Nurses assess blood pressure, review the patient's medical records, document lifestyle factors, including activity level, diet, and other habits, and inquire about any existing symptoms, such as dizziness or fatigue.
- Diagnosis: After gathering information, nurses define the main issues. Common examples might include decreased cardiac output related to hypertension or ineffective health maintenance related to poor understanding of medication.
- Planning: The nurse translates findings into goals, tangible, realistic ones, such as lowering blood pressure to within normal limits, building a consistent medication routine, etc.
- Intervention: The nurse tracks readings, teaches, encourages movement, and sometimes repeats the same advice in different words because that’s how learning sticks. A dietitian can join in, or a family can help with reminders. Every small interaction is important.
- Evaluation: And finally, the reflection. The nurse looks back at the goals, compares numbers, and listens to how the patient feels. The hypertension nursing care plan evolves with the patient’s progress, helping to maintain steady blood pressure and prevent complications.
Nursing Assessment
In a nursing care plan for hypertension, assessment means looking closely at how blood pressure affects the patient’s whole body and daily life. Nurses gather both what the patient says and what they observe during care. This first step helps shape every decision that follows.
Subjective Data (What the patient shares):
- Headaches, dizziness, blurred vision, or feeling tired
- Chest pain, strong heartbeat, or trouble breathing
- Medications taken, missed doses, or side effects
- Eating habits, salt use, and level of exercise
- Alcohol, caffeine, or tobacco use
- Sleep quality and possible sleep apnea
- Daily stress and routines that raise blood pressure
Objective Data (What the nurse measures or observes):
- Blood pressure readings taken in both arms and at different times of day
- Pulse, breathing rate, and temperature
- Weight, body mass index, and fluid retention signs
- Lab results such as blood urea nitrogen, creatinine, and complete blood cell count
- Possible organ changes, like reduced kidney function or vision problems
- Central and peripheral pulse strength and rhythm
For students learning to write structured plans, EssayPro offers step-by-step guidance on related topics like the nursing care plan for diabetes.
Nursing Diagnosis
A nursing care plan for hypertension helps nurses identify the primary issues associated with high blood pressure and provide care tailored to the patient’s specific needs.
1. Decreased Cardiac Output
- Cause: The heart rate is high because of high pressure or extra fluid.
- Signs: Tiredness, shortness of breath, weak pulse, or low oxygen.
2. Ineffective Health Maintenance
- Cause: The patient doesn’t fully understand how to manage hypertension.
- Signs: Missed pills, poor diet, or skipping blood pressure checks.
3. Risk for Decreased Kidney Function
- Cause: Long-term high blood pressure or diabetes.
- Signs: Less urine, swelling, or high creatinine and BUN levels.
4. Risk for Poor Brain Circulation
- Cause: Too much pressure in the brain vessels.
- Signs: Headaches, dizziness, confusion, or vision problems.
5. Lack of Knowledge
- Cause: Limited understanding of treatment or lifestyle changes.
- Signs: Questions about medications, diet, or what hypertension means.
Nursing Goals
When you write a nursing care plan for hypertension, you’re describing what better looks like for your patient in real, measurable terms. Goals are where the plan begins to take shape. They give everyone, from nurse to patient, a direction that feels possible.
There’s a familiar rule that you’ve probably heard a dozen times in nursing school - keep them SMART: Specific, Measurable, Achievable, Relevant, Time-Bound.
It works because it turns vague wishes into steps someone can actually follow. You can’t track 'get healthier,' but you can track 'maintain blood pressure below 130/80 mmHg for two weeks.' That’s something you can write down, talk about, even celebrate.
Short-term goals come first because they’re the quick confidence boosts everyone needs.
- The patient’s blood pressure will lower to a safer range within 48 hours of starting medication.
- The patient will repeat their medication schedule before discharge without hesitation.
Then come the long-term goals, the ones that stretch beyond the hospital stay.
- The patient will keep blood pressure within the normal range for at least three months through consistent medication use and lifestyle changes.
- The patient will follow a low-salt diet, track readings at home, and share results at follow-ups.
- The patient will name at least three ways to manage stress by the next clinic visit because stress, as simple as it sounds, really does sneak into everything.
Nursing Interventions
Interventions turn observation into action. Each section below breaks down a key focus area, including how nurses monitor the heart, support adherence, alleviate discomfort, and encourage lasting lifestyle changes that help maintain steady blood pressure.
Maintaining Cardiac Output and Tracking Blood Pressure
Every blood pressure check shows how the heart’s holding up. Nurses record readings at regular intervals, in both arms, with the patient sitting quietly. These numbers are clues. They reveal how well treatment works and when something starts to slip.
Sometimes the monitor appears fine, but the patient reports feeling dizzy, lightheaded, or off. Documentation bridges that space, giving shape to what can’t be measured by the cuff alone.
Monitoring also means watching for small warning signs: swelling in the legs, sudden headaches, blurred vision. These moments hint at complications, and catching them early matters more than anything else
Administering Medication and Supporting Understanding
Antihypertensive medications might help regulate the numbers, but only if used as directed. Nurses double-check the dose, administer the medications, the beta blockers and calcium channel blockers, and then assess for possible side effects, fatigue, dry cough, or swelling, to name a few. In the end, not to overanalyze every side effect, but again, patterns matter.
There’s a contradiction here worth naming: patients rely on medicine to stay safe, yet medication only works if they believe in it enough to take it daily. Nurses walk that fine line between instruction and encouragement. They explain the purpose behind each pill, the timing, and the need for routine. Some patients forget, while others become discouraged. The job is to make adherence feel possible.
Helping the Body Adjust to Activity
Hypertension can drain energy. Medication sometimes does the same. The body slows down before it strengthens again. This leads to Activity Intolerance, a nursing diagnosis that describes fatigue and breathlessness with effort.
The nurse’s task isn’t to push but to pace. Take a walk, then rest; try again later. Monitor vital signs before and after, and listen when the body says 'enough.' Progress shows in a longer walk, a shorter rest, and a steadier breath.
Meanwhile, if you ever find yourself thinking, ‘I wish someone could write my nursing research paper,’ EssayPro offers guidance that helps you write with the precision and tone real nursing work demands!
Managing Pain and Discomfort
High blood pressure has a way of reshaping pain. Headaches rise from the back of the neck, sharp and pulsing. Patients often downplay them, saying it’s 'just stress.' Still, those headaches can indicate increased cerebral pressure, which is a significant concern.
Under the nursing diagnosis of Acute Pain, the aim is to provide relief with awareness. Nurses encourage rest, quiet rooms, and slow breathing. Medication helps, yes, but comfort often starts before the pill, with turning off the light, easing conversation, etc.
Pain management is about reducing tension so the body can reset, and blood pressure follows suit.
Building Coping Skills and Encouraging Routine
Managing hypertension is a daily practice. Some patients follow every instruction, others drift. That’s where the nursing diagnosis Ineffective Health Maintenance comes in.
Nurses ask what’s getting in the way: Is it the cost of medication? The fatigue of taking care of everyone else first? Or the belief that a few missed doses won’t matter? Each answer helps nurses reshape the plan.
Effective approaches help shift intention into action. Nurses teach patients how to set up pill organizers or phone reminders, keep a log of readings in a notebook, and observe early warning signs when blood pressure is rising. They include family or caregivers in the conversation for support to make the habit easier to maintain.
Encouraging Healthy Habits and Lifestyle Shifts
Medication keeps hypertension under control, but daily habits determine how well it stays that way. Nurses play a central role in guiding these shifts, translating medical advice into everyday actions that make sense for each patient.
Nurses teach the DASH diet, explain how salt affects fluid balance, and emphasize the value of regular movement. They also promote simple movement routines. A short walk after meals, light stretching, or a few minutes of breathing exercises can do more for stability than people expect.
Weight control gets steady attention. Even modest loss lightens the heart’s workload. Stress management ties everything together. Nurses talk about breathing techniques, quiet moments, and setting realistic goals.
Hypertension Nursing Care Plan Template
This high blood pressure nursing care plan was designed to facilitate easy documentation of findings and tracking of progress. Use it as a guide when developing individualized plans for patients with elevated blood pressure.
Hypertension Nursing Care Plan Examples
To understand how the nursing process works in real practice, below are three examples of nursing care plans for hypertension. Each nursing care plan sample follows the ADPIE format.
This first example shows how a nurse might create a care plan for a patient with uncomplicated or primary hypertension. The focus here is on medication adherence, blood pressure monitoring, and lifestyle modification.
This sample of nursing care plan for hypertension focuses on a patient with both hypertension and Type 2 diabetes. The goal here is to improve blood pressure and glucose control through education, consistent monitoring, and medication adherence.
This plan addresses a patient experiencing a sudden, severe increase in blood pressure, a hypertensive crisis. Immediate intervention focuses on stabilizing vital signs, preventing organ damage, and teaching follow-up care.
Final Thoughts
A nursing care plan for hypertension ties all the moving parts of care together. It’s where monitoring, medication, and patient education meet in one steady rhythm. Creating this kind of plan takes time. There’s the data, the diagnoses, the interventions, and then the seemingly small details, like remembering how stress or skipped meals affect a patient’s pressure. These details build understanding and make the plan real.
For nursing students still learning the process, EssayPro is a reliable space to get professional help. Our authors will help you structure your thinking and translate clinical reasoning into solid written work.
FAQs
What Is the Nursing Care Plan for Hypertension?
A nursing care plan for hypertension is a written framework to organize assessments, diagnoses, and management for patients with hypertension. The care plan outlines goals, interventions, and the method for evaluating progress.
How to Write a Nursing Care Plan for Hypertension?
Start with assessment, which includes assessing the patient’s blood pressure, their history, and an overview of their daily routine. Based on the assessment, list the most significant problems (e.g., fatigue, poor adherence to medications) next. As the next step, include the interventions (e.g., checking vitals, teaching about timing medications or dietary changes, etc.). End with evaluation, what worked, what did not work, and what the next steps will be.
How Do I Decide on Nursing Diagnoses for a Hypertension Care Plan?
A diagnosis depends on what you find in your assessment. If the patient says, 'I am really tired after just mild activity,' then you should consider the diagnosis of activity intolerance. If the patient simply forgets to take their medications or does not follow up for their visits, it could be ineffective health maintenance.
How Many Nursing Diagnoses Can I Include in a Hypertension Care Plan?
There is no universal number of nursing diagnoses that should be included in a care plan, but 3-5 of the most important ones are usually sufficient to adequately address the issue leading to poor outcomes, without overwhelming the nursing care plan.
What Do You Write in a Nursing Care Plan Example?
A complete care plan example should show the whole process: assessment, diagnosis, goals, interventions, and evaluation. For hypertension, this might involve tracking blood pressure readings, identifying decreased cardiac output, setting a goal to reach normal limits, and outlining how the nurse will educate the patient about diet and medication.

Adam Jason
is an expert in nursing and healthcare, with a strong background in history, law, and literature. Holding advanced degrees in nursing and public health, his analytical approach and comprehensive knowledge help students navigate complex topics. On EssayPro blog, Adam provides insightful articles on everything from historical analysis to the intricacies of healthcare policies. In his downtime, he enjoys historical documentaries and volunteering at local clinics.
- Mayo Clinic. (2023, May 17). High blood pressure (hypertension) – Diagnosis and treatment. Mayo Foundation for Medical Education and Research. https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/diagnosis-treatment/drc-20373417
- Cleveland Clinic. (2024, January 3). Hypertension (high blood pressure). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/4314-hypertension-high-blood-pressure
- University of St. Augustine for Health Sciences. (2023, February 27). How to write a care plan: The ultimate guide. USAHS. https://www.usa.edu/blog/how-to-write-a-care-plan/




 (1).webp)

